 Overall breast cancer death rates dropped 39 percent between 1989 and 2015, averting 322,600 breast cancer deaths during those 26 years. And while black women continue to have higher breast cancer death rates than whites nationally, death rates in several states are now statistically equivalent, perhaps reflecting an elimination of disparities in those states.
Overall breast cancer death rates dropped 39 percent between 1989 and 2015, averting 322,600 breast cancer deaths during those 26 years. And while black women continue to have higher breast cancer death rates than whites nationally, death rates in several states are now statistically equivalent, perhaps reflecting an elimination of disparities in those states.
The findings come from Breast Cancer Statistics, published in CA: A Cancer Journal for Clinicians and its companion consumer publication Breast Cancer Facts & Figures, reports published every two years by the American Cancer Society to describe the latest trends in breast cancer incidenceIncidence refers to the occurrence of new cases of disease or injury in a population over a specified period of time., mortality, survival, and screening by race/ethnicity in the United States, as well as state variations in these measures.
Breast cancer is the most common cancer diagnosed among U.S. women (excluding skin cancers) with about 252,710 new cases expected to be diagnosed in 2017. It is the second leading cause of cancer death among women in the U.S., after lung cancer; 40,610 women in the U.S. are expected to die from this disease in 2017.
Eighty-one percent of breast cancers are diagnosed among women ages 50 years and older, and 89% of breast cancer deaths occur in this age group. The median age at diagnosis for all women with breast cancer is 62 years; the median age at diagnosis is younger for black women than for white women; and the median age at breast cancer death is 68 years overall (70 years for white women and 62 years for black women).
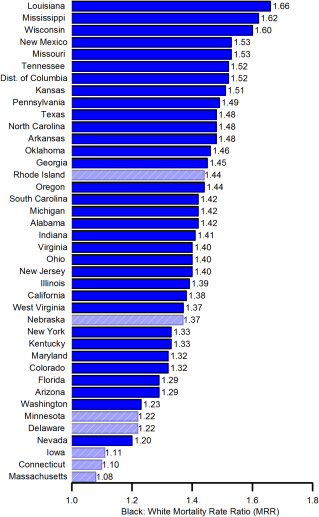
The report outlines substantial variations in breast cancer incidence and mortality rates by race/ethnicity in the United States. Non-Hispanic white (NHW) and non-Hispanic black (NHB) women have higher breast cancer incidence and death rates than women of other race/ethnicities; Asian/Pacific Islander (API) women have the lowest incidence and death rates. Although the overall breast cancer incidence rate during 2010 through 2014 was slightly (2 percent) lower in NHB women (125.5 per 100,000) than in NHW women (128.7 per 100,000), the breast cancer death rate during 2011 through 2015 was 42 percent higher in NHB women (29.5 per 100,000) than in NHW women (20.8 per 100,000).
The steep declines in breast cancer death rates since 1989 have been attributed to both improvements in treatment and early detection by mammography. By the same token, not all women have benefited equally from these improvements, as evidenced by variation in mortality trends. A striking divergence in long-term breast cancer mortality trends between black and white women emerged in the early 1980s and continued to widen over the last several decades, but recent data suggest that the racial disparity may be stabilizing.
In fact, while the excess death rate in blacks varies widely in the United States, ranging from 20 percent in Nevada to 66 percent in Louisiana, in seven states there were no significant differences in breast cancer death rates between NHB and NHW women. In many of those states, the closing gap may reflect a lack of statistical power (small numbers of breast cancer deaths among black women). But in Massachusetts, Connecticut, and Delaware, the similar rates suggest equitable breast cancer outcomes are achievable.
“A large body of research suggests that the black-white breast cancer disparity results from a complex interaction of biologic and nonbiologic factors, including differences in stage at diagnosis, tumorA mass of cells that can be benign or malignant. characteristics, obesity, other health issues, as well as tumor characteristics, particularly a higher rate of triple negative cancer” said Carol DeSantis, MPH, lead author of the report. “But the substantial geographic variation in breast cancer death rates confirms the role of social and structural factors, and the closing disparity in several states indicates that increasing access to health care to low-income populations can further progress the elimination of breast cancer disparities.”